The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
The Achilles tendon is a collection of fibrous tissues that connect the heel bone to the calf muscles. This tendon is responsible for our ability to walk, run, and jump, but it is very vulnerable to injury from athletic activities that put excess strain on the tendon. The three most common types of Achilles tendon injuries are an Achilles tendon tear, an Achilles tendon rupture, and Achilles tendonitis. An Achilles tendon tear, in which the tendon tears slightly, is characterized by intense pain, swelling, and difficulty moving the affected ankle. An Achilles tendon rupture, in which the tendon tears completely, may make a popping or snapping sound at the time of injury, cause severe pain, and make walking extremely difficult. Achilles tendonitis is an inflammation of the Achilles tendon. It usually causes burning pain in the calf and heel that intensifies during physical activity. If you have injured your Achilles tendon, it is suggested that you seek the care of a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Bruce Smit, DPM of Frankfort Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
 Diabetes is a disease that affects your blood sugar - so how can this condition affect the feet, too? The prolonged episodes of high blood sugar that are characteristic of diabetes often cause damage to the blood vessels throughout your body, including those that supply your lower limbs. Poor blood flow to the feet can lead to complications such as poorly healing wounds and a loss of sensation. Diabetes is associated with multiple conditions that affect the feet, including diabetic neuropathy, Charcot foot, peripheral artery disease, and gangrene. Signs of diabetes affecting the feet include swelling, tingling, numbness, weakness, skin discoloration, and foot wounds, among many others. If you have diabetes, it is suggested that you are under the care of a podiatrist, who can help you manage any foot-related symptoms.
Diabetes is a disease that affects your blood sugar - so how can this condition affect the feet, too? The prolonged episodes of high blood sugar that are characteristic of diabetes often cause damage to the blood vessels throughout your body, including those that supply your lower limbs. Poor blood flow to the feet can lead to complications such as poorly healing wounds and a loss of sensation. Diabetes is associated with multiple conditions that affect the feet, including diabetic neuropathy, Charcot foot, peripheral artery disease, and gangrene. Signs of diabetes affecting the feet include swelling, tingling, numbness, weakness, skin discoloration, and foot wounds, among many others. If you have diabetes, it is suggested that you are under the care of a podiatrist, who can help you manage any foot-related symptoms.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Bruce Smit, DPM from Frankfort Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
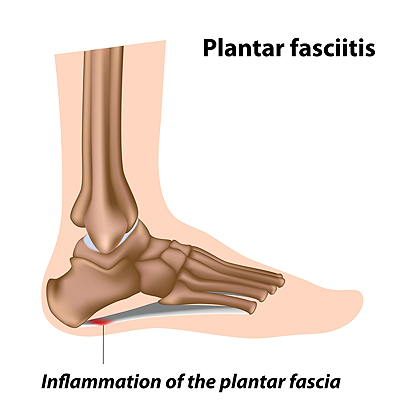 Plantar fasciitis is a condition in which the plantar fascia, a ligament that runs along the bottom of the foot, becomes injured, inflamed, and painful. Plantar fasciitis has a variety of causes, including spending too much time on your feet, engaging in high-impact repetitive activities like running, and wearing improper shoes that do not adequately support the foot. Plantar fasciitis can be treated conservatively by taking nonsteroidal anti-inflammatory medications to manage pain, stretching the feet each day, resting the feet regularly, massaging the feet, and wearing comfortable, supportive shoes. If you have plantar fasciitis, it is recommended that you see a podiatrist for treatment.
Plantar fasciitis is a condition in which the plantar fascia, a ligament that runs along the bottom of the foot, becomes injured, inflamed, and painful. Plantar fasciitis has a variety of causes, including spending too much time on your feet, engaging in high-impact repetitive activities like running, and wearing improper shoes that do not adequately support the foot. Plantar fasciitis can be treated conservatively by taking nonsteroidal anti-inflammatory medications to manage pain, stretching the feet each day, resting the feet regularly, massaging the feet, and wearing comfortable, supportive shoes. If you have plantar fasciitis, it is recommended that you see a podiatrist for treatment.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Bruce Smit, DPM from Frankfort Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
How Can It Be Treated?
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
 Stubbing your toe into a piece of furniture or dropping a heavy object on it are common ways to get a toe broken. It is often immediately noticed, and symptoms can include bruising, swelling, and difficulty walking. Minor fractures are treated by using the buddy taping method, which is accomplished by taping the affected toe to the toe next to it. An X-ray is generally performed to determine the severity of the broken toe, and it often takes approximately six to eight weeks to heal. If the break is severe, the bone may need to be pushed back into place, or surgery may be necessary for proper healing. If you have broken your toe, please speak with a podiatrist as soon as possible.
Stubbing your toe into a piece of furniture or dropping a heavy object on it are common ways to get a toe broken. It is often immediately noticed, and symptoms can include bruising, swelling, and difficulty walking. Minor fractures are treated by using the buddy taping method, which is accomplished by taping the affected toe to the toe next to it. An X-ray is generally performed to determine the severity of the broken toe, and it often takes approximately six to eight weeks to heal. If the break is severe, the bone may need to be pushed back into place, or surgery may be necessary for proper healing. If you have broken your toe, please speak with a podiatrist as soon as possible.
Broken toes may cause a lot of pain and should be treated as soon as possible. If you have any concerns about your feet, contact Bruce Smit, DPM from Frankfort Foot & Ankle Clinic. Our doctor will treat your foot and ankle needs.
What Is a Broken Toe?
A broken toe occurs when one or more of the toe bones of the foot are broken after an injury. Injuries such as stubbing your toe or dropping a heavy object on it may cause a toe fracture.
Symptoms of a Broken Toe
Although the injured toe should be monitored daily, it is especially important to have a podiatrist look at your toe if you have severe symptoms. Some of these symptoms include worsening or new pain that is not relieved with medication, sores, redness, or open wounds near the toe.
If you have any questions, please feel free to contact our office located in Frankfort, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.